Who Should Consider an Oophorectomy?
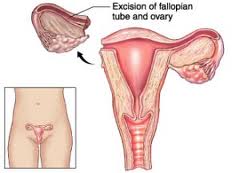
The term oophorectomy refers to the surgical removal of both the ovaries from a woman’s body. It can also include removal of the fallopian tubes, which is then called a salpingo-oophorectomy. But why would one want to remove such important organs? If you have a look at the articles on the BRCA1 and BRCA2 genes you can see that having a mutation in either of these genes significantly increases the risk of developing ovarian cancer (as well as breast cancer and fallopian tube cancer).
Therefore women who have confirmed genetic mutations in BRCA1 or BRCA2 have the option of undergoing an oophorectomy to reduce their chances of developing ovarian cancer. Usually women who are 35 years or older and have completed their childbearing are candidates for this surgery. Women who have strong family histories of ovarian cancer but do not have a mutation or choose not to have genetic testing can also consider having this procedure. Because the surgery is done to prevent cancer development, it is called a prophylactic oophorectomy (or salpingo-oophorectomy).
How much can an oophorectomy reduce the risk of cancer?
If you have a BRCA1 or 2 mutation, having this surgery can actually reduce your risk of both breast and ovarian cancer. For breast cancer, the risk can be reduced by up to 50% in premenopausal women. For ovarian cancer the risk can be reduced by 85% or more.
The risk of breast and ovarian cancer varies quiet a bit in studies. And your individual risk might vary depending on various factors such as your family history, lifestyle choices and other measures you take to prevent cancer. So for some women the benefits of having this surgery will be worth having it, while for others the risks and potential side effects may be too great to warrant the reduction in risk.
What are the risks associated with oophorectomy?
Generally this is quiet a safe procedure carrying a small risk of complications such as infections, intestinal blockage or injury to internal organs.
The major issues with this surgery are the complications that come from the loss of hormones that are made by the ovaries. For premenopausal women, having an oophorectomy causes them to undergo early menopause, which causes a number of side effects such as:
- Bone thinning (osteoporosis)
- Hot flushes
- Vaginal dryness
- Sexual problems
- Sleep disturbance
- Increased risk of heart disease
In addition to these, there is also a lingering risk of cancer development in the form other gynecological cancers or primary peritoneal carcinoma, which acts and looks just like ovarian cancer. The risk of this type of cancer is very low, much lower than the lifetime risk of ovarian cancer if the ovaries are intact. In one study, fewer than 1% of BRCA1 mutation carriers who underwent prophylactic surgery developed any kind of
What are the alternatives to oophorectomy for preventing ovarian cancer?
Prophylactic surgery is by far the most effective way of reducing ovarian cancer risk in high-risk women. So most doctors will recommend the surgery, but there are other options you could talk to your doctor about.
One option is increased screening for ovarian cancer. You may choose to have screening tests done twice a year to look for early signs of cancer. This usually includes a blood test for CA-125 and an ultrasound of your ovaries. This option has had some success in detecting ovarian cancer in its early stages, however the benefit in screening large populations has yet to be established.
Another option is to take birth control pills. Many studies have shown that contraceptive pills reduce the risk of ovarian cancer. Some of these also suggest a reduction in risk for high-risk women. There is some concern that the risk of breast cancer may increase in these women by taking birth control pills, but the benefits of reducing ovarian cancer seem to outweigh the small risk of breast cancer.
Should I take hormone replacement therapy after having an oophorectomy?
The use of low-dose hormone replacement therapy after oophorectomy is controversial. Some studies suggest that hormone therapy may increase the risk of breast cancer and endometrial cancer, while others suggest that early menopause itself can cause its own serious risks.
Up to the age of 45, a woman who undergoes this type of surgery and doesn’t use hormone replacement therapy has a higher rate of premature death due to cancer, heart disease and neurological disease. Doctors typically recommend that younger women who have their ovaries removed consider low-dose hormone replacement therapy until the age of 45 or 50.
There is no conclusive evidence as to what effect hormone therapy has on cancer risk. If you decide to take low-dose estrogen, it is a good idea to stop taking it after the age of 50. In any case, you should consult with your doctor as to the risks and benefits particular to your individual situation. There is the option of having your uterus removed during the prophylactic surgery. This will allow you to take a form of hormone therapy which may be safer for women with a high risk of breast cancer, but removing the uterus (called hysterectomy) is also controversial.
As you can see, there are many things to consider when thinking about having prophylactic oophorectomy. The decision is a challenging one and has no right or wrong answer. It comes down to a personal choice only you can make. Advice from a genetic counselor or a gynecologic oncologist can help you make a more informed decision.